As we soak up the sun this summer, it’s essential to balance enjoyment with skin protection, especially for seniors who face increased risks of skin cancer. Did you know that UV rays from the sun are the primary cause of skin cancer? But fear not! With practical tips and understanding Medicare coverage, you can stay safe and enjoy sunny days responsibly.
Protecting Your Skin: Practical Tips
- Seek Shade Strategically During peak sun hours (10 a.m. to 4 p.m.), find shade under an umbrella, sunshade, or in shaded areas to reduce UV exposure. It’s your personal oasis from the summer heat.
- Fashionable Sun Protection Stay stylish and sun-safe with loose, breathable clothing, a wide-brimmed hat, and UV-blocking sunglasses. Protect yourself from head to toe while looking your best.
- Sunscreen: Your Skin’s Superhero Always apply broad-spectrum sunscreen with SPF 30 or higher. Reapply every two hours (more frequently if swimming) and opt for waterproof formulas for continuous protection.
- Embrace Vitamin D Wisely Maintain strong bones with vitamin D-rich foods like salmon and dairy products. Consult your doctor about supplements for additional options beyond sun exposure.
- Review Your Medications Certain medications can increase skin sensitivity to sunlight. Discuss your prescriptions with your healthcare provider to stay informed and protected.
- Stay Cool and Hydrated Beat the heat by staying hydrated and wearing lightweight, breathable fabrics. Moisturize regularly to keep your skin healthy and hydrated.
Early Detection Saves Lives
Monitor your skin for changes such as unusual moles or patches. Promptly notify your doctor if you notice anything concerning – early detection is crucial for effective treatment.
Understanding Medicare Coverage for Skin Cancer
The senior population faces significant risks from skin cancer, with over 40% of melanoma cases in the U.S. occurring in those aged 65 and older. Here’s how Medicare supports your skin health:
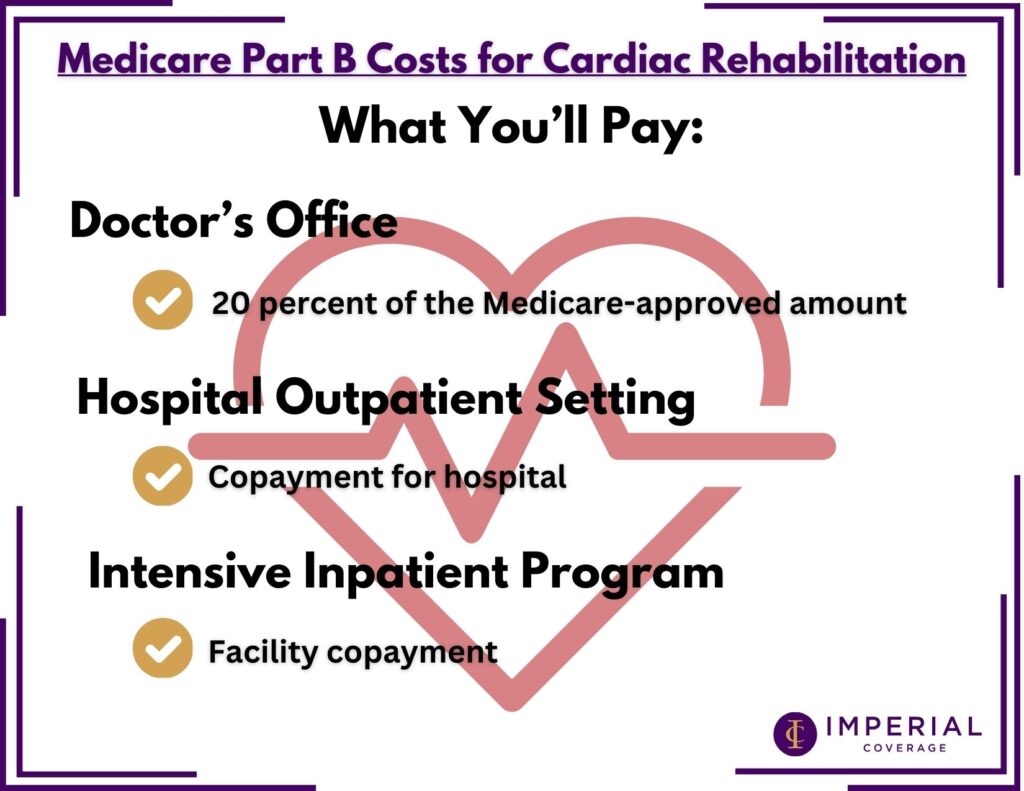
- Medicare Part B Coverage
- Routine skin cancer screenings are not covered for asymptomatic individuals under Medicare Part B.
- Medicare Part B covers doctor examinations if you notice changes in moles or skin growths. If further evaluation is needed, Medicare may extend coverage for specialist referrals.
- Coverage for Treatment
- Medicare Part A and Part B cover outpatient treatments for skin cancer after meeting deductibles. Hospitalization costs are covered under Part A after its deductible is met.
- Annual Wellness Visits
- Medicare Part B offers annual wellness visits, providing an opportunity to discuss skin health concerns with your doctor. The visit is covered without applying the Part B deductible.
- Medicare Advantage and Prescription Coverage
- Medicare Advantage plans cover the same benefits as Original Medicare (Part A and B) and may offer additional coverage options.
- Medicare Part D plans cover prescription drugs used for skin cancer treatment, expanding coverage beyond Original Medicare’s limitations.
Whether you’re considering Medicare Advantage or need comprehensive coverage insights, exploring your options ensures you receive the best care for your skin health needs. Stay informed, stay protected, and enjoy the sunshine responsibly this summer!
If you have further questions about your Medicare coverage, or would like to schedule a plan review, please contact our customer support services.